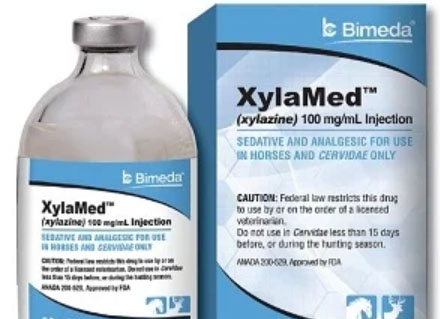
XYLAZINE / Tranq
A powerful sedative that the FDA has approved
for veterinary use only
Know what’s in your drugs
Xylazine is a non-opioid drug that can slow down the nervous system. It can make breathing and heart rate slower. When tranq is mixed with another drug like heroin, fentanyl or a benzo, it can increase the risk of overdose. The Biden-Harris administration designated fentanyl combined with xylazine as an emerging threat to the United States.
In case of overdose, here’s what you can do:
- If you think someone has overdosed, give them NARCAN®* and call 9-1-1.
- If the person is not responding, check if they are breathing.
- If the person is not breathing and not responding, provide rescue breathing (1 breath every 5 or 6 seconds).
- If the person starts breathing again (10 breaths/minute), but still seems sleepy, gently move them into a rescue position and keep a close watch on them.
* While xylazine doesn’t respond to NARCAN®, opioids do, so please try it.
Tranq has been linked to serious wounds that can quickly get worse and spread.
Tranq, whether smoked, snorted, or injected, can cause serious wounds that may need medical attention. It’s important to see a doctor promptly if you have a wound from using tranq, and to keep it clean and covered to avoid infection.
What can you do if you think there is tranq in your drugs?
Before buying or using a drug, ask others how it makes them feel. Tranq can make you really sleepy, so if you are using it, be sure to use it in a safe place where you won’t fall and hurt yourself. If you think there’s tranq in your drugs, tell someone at a local exchange program so others can be careful too.
You can purchase xylazine test strips here.
Frequently
Asked
Questions about Tranq / Xylazine
Related Posts

Only 1 in 4 Adults Needing Opioid Use Disorder Treatment Received Medications
Black and Latino adults less likely to receive any treatment by Shannon Firth, Washington Correspondent, MedPage Today June 27, 2024 Only about a quarter of adults who needed treatment for opioid use disorder (OUD) received recommended medications, survey data showed. In 2022, the National Survey on Drug Use and Health (NSDUH) found that 3.7% of…

OD Free Marin Presentation to Marin Board of Supervisors for 2024 National Fentanyl Awareness Day
Please view the 2024 National Fentanyl Awareness Day commemoration (starts at 54:46 minutes into the Marin Board of Supervisors’ meeting on 5/7/24.) This segment (#4 in the agenda) includes updates from Supervisor Katie Rice (who sponsored the resolution) and Public Health Officer Matthew Willis, MPH, MD, as well as input from interns, the community and…

2024 Community Forum – Video
If you were unable to attend our online community forum on April 10th, here is a replay of the event in full. Learn about best practices, available resources, spotlight innovative efforts underway, and engage attendees in helping to end overdoses in Marin. Together, we are working to prevent overdose and improve the health and well-being…
